In a recent statement from the National Catholic Bioethics Center on COVID-19 vaccines, we noted that the Catholic Church “neither requires nor forbids” the use of vaccines, but instead urges people to “form their consciences and to carefully discern the moral and prudential issues involved.”
A 2020 Vatican statement offers a similar conclusion: “vaccination is not, as a rule, a moral obligation,” and “therefore, it must be voluntary.”
That’s why, when Catholic colleges and universities mandate COVID-19 vaccines as a condition for enrollment, as several have recently done, important ethical conflicts and prudential concerns arise.
Vaccine mandates run counter to the wisdom of encouraging individuals to make careful and case-specific determinations regarding their personal health needs. Such mandates bolster the idea that the judgment of a higher authority, say a university president or a politician, should be substituted for their own free and informed consent.
In general, when I become sick, I ought to function as the decision-maker regarding my medical treatments, even as I work closely with my health care providers to receive the information I need to make the best decision. Similarly, if I am healthy, but face the risk of exposure to a new disease, I must weigh the benefits and burdens of prophylactic measures like vaccines.
Early in a pandemic, there can be a lot of questions and uncertainty because of shifting sets of medical data or a growing sense of alarm and panic. We may be tempted to think we can or should sideline ethical or prudential concerns.
Yet it is at precisely such a time that our ethics and prudential judgments become paramount, as we seek to temper urgency with due diligence, and to confront our fears with reason and discernment. It is in such a crisis moment that calm, careful, and case-by-case discernment becomes crucial.
Mandating vaccines for everyone involves a flawed assumption that there are only benefits, and no significant burdens, associated with getting vaccinated. The history of vaccine development reminds us how vaccines, which constitute a breakthrough technology and life-saving remedy in the battle to improve public health, are nevertheless not a risk-free endeavor.
Some individuals have allergies to vaccine ingredients. Others have immune systems that cannot tolerate vaccines. Some vaccine recipients encounter unanticipated reactions and side effects, whether it’s headaches, muscle aches, several days of exhaustion or nausea, anaphylaxis or the rare blood clots seen among those who received the Johnson & Johnson COVID-19 vaccine.
When deciding about vaccinations, other considerations besides safety and side effects also come into play.
There are ethical concerns about the way certain COVID-19 vaccines are connected to cell lines derived from abortions.
Certain populations, statistically speaking, will face low risk from diseases like COVID-19, including otherwise healthy college-age students and children, many thousands of whom have tested positive but most of whom have experienced only mild symptoms or may have been entirely asymptomatic. Those who have been previously exposed to COVID-19 may decide to delay or decline vaccination, since they already have acquired some immunity.
For those, meanwhile, who are more vulnerable to the coronavirus and its potentially damaging effects, like those who are elderly, obese, diabetic, or facing other comorbidities, it makes sense for them to consider the potentially safer path of vaccination, rather than risking a harmful (or deadly) encounter with the virus itself. The same would hold for young people who are obese or diabetic, or have regular contact with vulnerable groups like the elderly.
Finally, mandates can sometimes have an effect opposite to what is intended. People can stubbornly dig in their heels when certain behaviors are compelled.
Jonah Berger, a marketing professor at the Wharton School has noted that there is some evidence that telling people what to do can backfire, as with “Just Say No” style anti-drug campaigns that may actually increase drug use among certain subgroups of young people.
“People want to feel like they’re in control of their choices,” Berger says.
He notes, however, that once people have described what they care about and believe others have addressed those concerns, it’s much harder for them to push back merely for the sake of resisting: “They’re [now] a participant in the process rather than being forced to do something.”
Especially at Catholic universities and colleges, where we are seeking to form the next generation of society’s leaders and thinkers, instead of imposing the requirement to get vaccinated, leaders would do better to share and explain to students the benefits and risks of vaccinations — scientific and ethical — to help them decide.
By offering evidence-based information and moral principles, rather than mandates, college students will be helped to clarify their own processes of intellectual and personal discernment, and acquire the habit of making more prudent and informed choices.
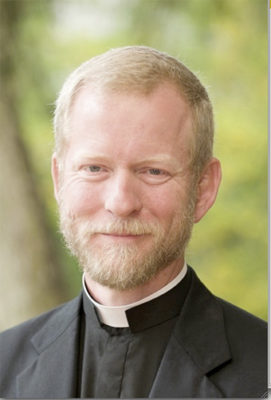
Fr. Tadeusz Pacholczyk, Ph.D. earned his doctorate in neuroscience from Yale and did post-doctoral work at Harvard. He is a priest of the diocese of Fall River, Massachusetts, and serves as the director of education at The National Catholic Bioethics Center in Philadelphia. See www.ncbcenter.org and www.fathertad.com.